First, the patient, second the patient, third the patient, fourth the patient, fifth the patient, and then maybe comes science. We first do everything for the patient; science can wait, research can wait
— Béla Schick (1877–1967)
As early as 1972, a study reported that the usage of a computerised medical decision support system surpassed the diagnosis capability of the most senior physician. Using Naive Bayes’ Theorem, the probability of an AAP (acute abdominal pain) disease is calculated.
While the AAPHelp system reported an accuracy of 91.8% in diagnosing a patient with the correct disease, the most senior physician achieved only 79.6%. In 1986 another study involving almost 17.000 patients, showed that the initial diagnostic accuracy increased from 45.6% to 65.3% after the AAPHelp was introduced. As a result, the mortality rate dropped by 22%. All in all, the AAPHelp system showed incredible potential and implementing it in healthcare could only be seen as a natural next phase.
Nowadays, Artificial Intelligence (AI) is able to contribute to the diagnosis, prognosis and development of a treatment protocol for a patient by using machine learning. Pattern recognition techniques, trained on thousands of cases, are able to attain high prediction accuracies comparable to physicians.
So if I were to walk into a hospital tomorrow with acute pains in my stomach, I would certainly be diagnosed, treated and cured by a smart algorithm, right? However, nothing could be further from the truth than this scenario. Some of the key obstacles that prevent the application of AI in the medical world are limited training data for certain health problems, privacy issues and distrust towards machines. We have known for almost 40 years how AI supported diagnoses are able to surpass human judgment, but our feelings towards this can be described as ambivalent. Nevertheless, the positive sides of AI in medical diagnosis, which include, the mitigated mortality rate, the cost-effective care and the expert-level accuracy are irrebuttable. In this article we will plead why using AI in medical diagnosis would be beneficial to the patient, physician and hospital.
Where Are We Now?
The health system plays a pivotal role in population health and can be directly influenced by the machinery of government. According to the World Health Organization (WHO), public expenditure is showing diminishing returns due to serious organizational inefficiencies, mistakes in health intervention and tremendous waste of resources. Computation has shown to be able to assist in resolving all of these issues, but AI-based methods in particular hold great promise. Artificial intelligence has revolutionized many fields, ranging from natural language processing to computer vision. With the ever-increasing rate of patient data digitalization, along with substantial increases in computing power, AI is starting to profoundly transform the way we practice healthcare as well.
Histopathology is a domain of particular interest, due to many inherent difficulties associated with the diagnostic process. It is at these fringes where the value of AI becomes most apparent. Consider oesophageal cancer, which is typically diagnosed in a late stage and has a bad prognosis. Barrett’s oesophagus (BO) is the only known precursor to oesophageal cancer and is a strong indicator for malign transformation. Early detection of BO can increase patient survival, for which microscopic tissue examination is necessary. The absence of objective directives for microscopy interpretations lead to unacceptable under- and overtreatment.
This is best exemplified by a recent study. A key takeaway is that even among pathologists there exists diagnostic variation. First, the researchers gathered 55 widely varying BO biopsies. They then drafted four expert pathologists, characterized by their extensive experience in BO dysplasia assessment, to set a golden standard evaluation. Then, 51 heterogeneously selected reference pathologists were asked to classify the same biopsies, such that the level of concordance could be determined. Results showed that overall concordance was only 60.66%.
Another study emphasizes that histological images can be taken at different scales and that pathologists analyse tissue samples at varying magnification levels. The reason for this is that there are multiple features that contribute to various stages of cancer and each of these features is best appreciated at different zoom levels. For instance, the structural configuration of cells is best appreciated at a lower zoom level than the anatomy of individual cells. At first glance this appears to be methodologically solid, but when one considers that every pathologist has her own magnification preferences, severe variance starts to enter the picture. As a result, regulations require diagnoses to include a second opinion from expert pathologists, but this does not completely resolve the variability issue. All in all this stresses the urgency to have a computational evaluation method, such that we can objectively and reliably assess disease progression.
AI-based methods are especially suited for this task when there is sufficient tissue data available. The more data there is available, the more accurate and reliable these models will be. Interestingly, this data is not restricted to tissue samples. In fact, the entire medical history, such as age, gender, blood pressure and smoking history can all be included for AI models to learn from. This not only makes the models more accurate. But also sets up for personalized treatment plans.
Besides this, AI also guarantees rapid diagnosis. It is currently the case that pathologists manually annotate tissue samples, which can take up to several hours per sample and this is aside from the loss of accuracy when fatigue sets in. Having machines take over this task such that pathologists only need to play the role of overseer, will reduce workload and free up more time for valuable doctor-patient interaction.
In light of the foregoing, it is expected that one day AI-based computational pathology will reduce unnecessary interventions, which in turn will therefore improve the quality of life for patients and make the health system more economical. Furthermore, AI is also expected to reduce underdiagnosis, meaning patients will more often receive treatment at the right time. When it is the case that diagnoses are more accurate and appropriately timed, patients on the whole will spend less time in the health system. This means that waiting lists will shrink and that patient throughput is increased.
But most importantly, AI models are not disease specific. Once a new model is established, it can be retrained to be applicable to many other diseases, given that the data is of the same form. For example, models that work on digitalized images of the oesophagus tissue samples will also be applicable to images of the liver tissue when retrained on that data.
Factors like an ageing population, reduced workload for doctors and national goals to expand care accessibility, make for an increased demand for physicians. One way of solving this ever-growing need could be to let an AI take over tasks of the physician. By applying pattern recognition, an AI is able to read off X-rays, CT, PET and MRI scans to detect diseases and diagnose patients. However, instead of diminishing the need and value of physicians, AI has the potential to augment the accuracy, efficiency and value of the physicians’ work. While the AI performs routine tasks, the doctors are able to spend more time with the patient, resulting in increased patient satisfaction. Especially in remote places where physicians are hard to come by, a time-saving AI device could really tilt the scales towards a more efficacious and improved healthcare system.
The Death of Bedside Medicine?
Thus far we have seen that applying AI in healthcare could relieve the shortage of medical staff and enable physicians to spend more time with their patients, resulting in increased patient satisfaction. In combination with factors like rapid diagnoses, personalized treatment plans and the general applicability of AI should be enough for the medical world to ensure that AI is used inside the hospital as soon as possible, right? However, this new technology is not welcomed with open arms inside the hospital. Attitude towards the use of AI could be described at best as skeptical, at worst as hostile.
Based on our discussion in the previous section it would appear that the success of AI stands or falls with data availability, and that brings us to a glaring problem. Extensive regulation is in place to protect patient data, meaning it is not directly available to researchers which stifles scientific progress. On the other hand this is a blessing. When a doctor makes a mistake, it only affects the one patient under his care, but when a widely used flawed algorithm makes a mistake, the damages could be incalculable. Moreover, these regulations give some assurance that a patient’s history does not end up in the hands of insurance companies with all that this implies for those individuals.
Patients are reluctant in accepting care provided by AI’s, concerned that their unique circumstances, symptoms and characteristics will be neglected. Given the superior accuracy that AI’s display, common sense would dictate that we should have AI’s assist physicians. Yet, it seems as though this is not easily accepted by patients, who believe that machines are only capable of standardized tasks, and every patient is screened, diagnosed and cared for in the same way. However, as we have stated previously, due to the personalized treatment plans, the AI is able to draw up a unique analysis for each patient. Healthcare providers should emphasize more on the personalized care that AI could deliver, for example through personalized feedback (“based on your unique profile…”). Changing this belief would be fundamental towards the acceptance of AI in the medical world and reaping the full benefits of artificial intelligence.
This reluctance in accepting the aid from AI is not only seen within patients, but can be perceived under physicians as well. Experts fear that AI will supersede human physicians, making medicine, one of the most prestigious and sought-after studies, possibly not so future-proof after all. This reluctance comes from the inaccurate fear that AI will make physicians redundant and will—aside from taking over lower skilled jobs—also threaten the jobs of people with a higher educational level. However, this fear is nonsensical. As previously mentioned, there is an ever-increasing demand for physicians and AI will mostly erode the repetitive tasks, enabling more patient-doctor interaction. And although AI is extremely good at regurgitating facts and achieving expert-level diagnoses, breaking bad news to a patient as well as critical or creative thinking is still reserved for the human physicians. The view of technology vs. humans should be put to an end since the new innovations strive to improve and augment healthcare. The convergence between AI and healthcare could be extraordinarily fruitful, with AI supporting the physicians in every way possible with the never-ending computing power and precise accuracy and the physicians lifting the patient care to a higher level. It should become common practice for physicians to be educated on how to benefit from all the things AI has to offer. With suitable and timely training, the reluctance under physicians can be subdued, enabling them to focus on scaling up the quality of hospitalized care.
My Perfect Pocket Doctor
In addition to AI surfacing inside the hospital doors, AI in healthcare is also arising inside people’s homes. Self-diagnosing apps like Symptomate, Ada and Diagnose en Behandeling assist in the process of diagnosis and bring the hospital to the patient. With Ada having 5+ million downloads, a rating of 4.7 stars in the Google App Store and reviews such as “Almost always accurate”, “GOOD ASSESSMENT”, and “Handig om te bekijken wat je evt mankeert zonder dat je er voor naar de dokter/ ziekenhuis moet,” it seems as though the general public has taken a liking to the AI doctor inside their smartphone.
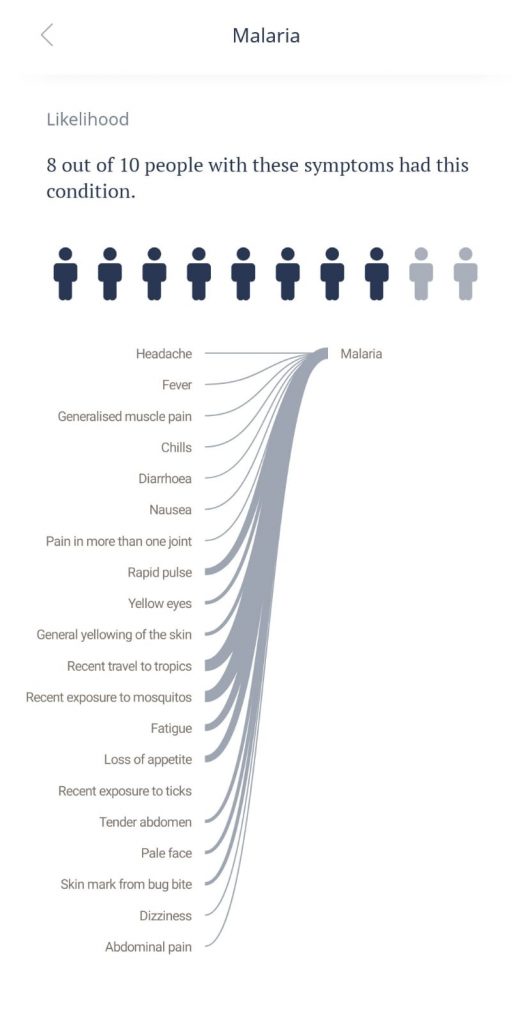
But does this app really recognize the disease when presented with the symptoms of its user? We decided to try out Ada for ourselves to see how accurate she really is in diagnosing our serious case of malaria. And within 10 minutes, Ada urges me to seek emergency care, because 8 out of 10 people with these symptoms had malaria. It seems as though the hype around Ada was justified, that maybe we should get rid of hospitals and physicians altogether, replacing them with self-diagnosing apps instead.
Scientific literature disagrees, stating that only 34% of the symptom checkers give the correct diagnosis in comparison to 72% of the trained physicians. And although Ada was accurate in predicting our malaria case, with a less distinct, clear-cut disease, she might not be as successful. Experts admit that it is more realistic for symptom checkers to assist physicians in their practice, than for individual use at home. The pocket-sized doctor inside your smartphone still seems like it has a long way to go, righteously so.
Doctor Who? Doctor Robot?
In the foreseeable future, hospitalized care will be even more centered around data. Artificial intelligent algorithms will support the diagnoses, personalized treatment plans and prognoses of patients. However, instead of fear, this progress should be met with enthusiasm. By supporting physicians and reducing their routine tasks, AI has the potential to augment physicians and the care they provide. AI fundamentals should be an integral part of physicians education and healthcare providers should urge their patients that they would only benefit from the care that AI’s provide. Self-service in healthcare does not yet seem around the corner though. Self-diagnosing apps like Ada do not provide a reliable diagnosis and should—for now at least—be sidelined. With similar spirit as Béla Schick’s sentiment, AI can put the care back into healthcare. The patient’s health should always be central, the way it is supposed to be.